According to the 2019 Malaysian National Cancer Registry, there are more than 700 newly diagnosed cases of cervical cancer per year in Malaysia and at least 40% were detected in stages 3 and 4.
The Malaysian Oncological Society in collaboration with Rose Foundation, National Cancer Society Malaysia, Majlis Kanser Negara (MAKNA), All Women’s Action Society (AWAM) and Women’s Aid Organization (WAO) are organizing a two month social media campaign to raise awareness of cervical cancer, screening and HPV vaccinations among Malaysian women. Critical to the success of this campaign is the active involvement of our social media champions to spread the message far and wide among their followers.
- Vaginal bleeding after intercourse, between periods or after menopause.
- Watery, bloody vaginal discharge that may be heavy and have a foul odor.
- Pelvic pain or pain during intercourse.
If you are having these signs and symptoms, immediately make an appointment with your gynaecologist for further assessment.
The survival rate is close to 100% when precancerous or early cancerous changes in the cervix are found and treated. Stage 1, 2, and 3 cervical cancer can be cured with early treatment.
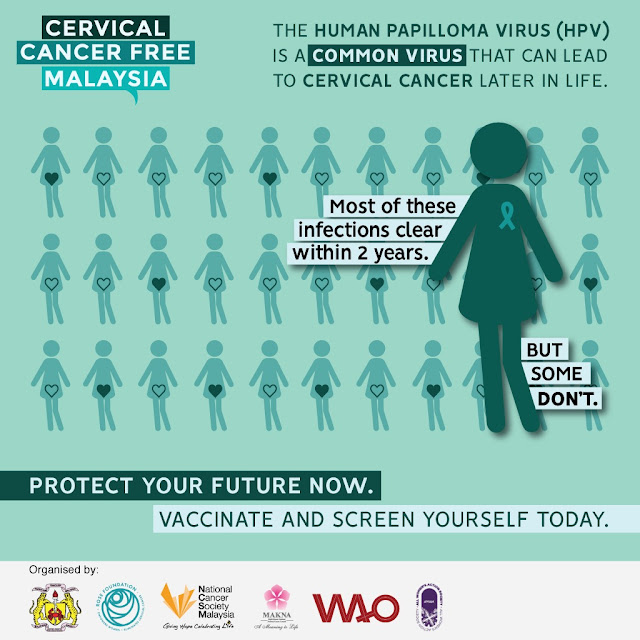
Human papillomavirus (HPV) is the most common viral infection of the reproductive tract. There are more than 100 types of HPV but only 14 types cause cancer. More than 95% of cervical cancer is caused by persistent infection by these HPV types.
The human papillomavirus (HPV) is spread through genital skin to skin contact usually during sex. Most HPV infections disappear within the first 2 years but for some (without HPV vaccination), the virus will last longer in the body. It takes up to 10 years to convert healthy cervical cells into cancerous cells.
HPV vaccination and regular cervical screenings are two important methods to prevent cervical cancer.
The HPV vaccine prevents new infections by the common types of HPV that can cause cervical cancer. It does not treat existing HPV infections or disease.
HPV vaccination is most effective in early adolescence and must be given in a series of shots. It is recommended for both boys and girls:
- Between 9 – 14 years old (2 shots: 1 shot after 6 months)
- Between 15 – 26 years old (3 shots: to match-up the effectiveness of early adolescence HPV vaccine.
- Women above 26 years old are advised to speak to doctors to consider the vaccine.
The HPV vaccines have been available in Malaysia since 2006.
In 2010, a school-based HPV immunisation programme was implemented nationwide and since then, all 13-year-old girls receive the HPV vaccination in Malaysia (first year of secondary school).
The HPV vaccination trains your body’s immune system to detect and eliminate HPV early on in the infection so that the virus does not persist in the body.
Persistent HPV infection can lead to pre-cancerous changes in the cervix which can turn into cancer.
The HPV vaccine is safe and has significantly reduced the rates of cervical pre-cancer in women.
Some of the side effects of this vaccine are fever, fatigue, headache and redness or swelling of the skin where the vaccine was given but people recover quickly.
HPV vaccines are widely available in Malaysia.
Find a clinic or a hospital closest to you and make an appointment now to get your HPV vaccination.
The HPV vaccine only prevents infection from the main types of HPV that causes most cervical cancers.
Regular cervical screening is strongly advised to detect cervical cancer caused by less common types of HPV.
No, HPV vaccination can only prevent new infections.
It is not effective in treating people who have already been infected. Therefore, regular cervical screening is necessary.
Women who have ever engaged in sexual activity, between ages of 30-65-year-old, regardless of their marital or menopause status should get screened and follow the recommended cervical screening schedule.
Screening is a part of the comprehensive approach to cervical cancer prevention and control.
It is especially recommended to women without symptoms because cervical cancer generally only manifests its signs when it has reached a later stage. If an abnormality or early cancer is detected during the screening, it can easily be treated.
Cervical cancer develops from abnormal cells that can grow without any symptoms for several years. Screening at regular intervals is vital to detect these abnormal cells before they become cancerous.
You should do a screening test that you are comfortable with, once meeting its eligibility criteria.
Two cervical screening tests that help prevent cervical cancer are pap smear and HPV test. Pap smear is conducted by a healthcare professional to detect abnormal cell changes for women between ages 21 to 65 years old, who have engaged in sexual activity; whereas an HPV test can detect oncogenic HPV types which are the causative agent of abnormal cell changes. With a sensitivity rate of more than 90% (Pap smear is around 50%), HPV test is recommended for women aged 30 to 65 regardless of their marital or menopause status and could be performed by the patient themselves.
Yes, you can choose to.
The HPV test is a more sensitive cervical screening test and a negative test result would mean that you would not need to undergo cervical screening for the next 5-10years (if you are aged between 30 to 65 years old).
Pap smear: Repeat once every 3 years if the first two consecutive years’ test results are normal.
HPV Test: Repeat it once every 5-10 years if you are tested negative.
*Within a span of 10 years, a patient with a normal result would have taken 2 HPV tests or 4 pap smears.
- You are aged between 30 – 65 years old
- You are not pregnant
- Never had a hysterectomy (removal of your womb)
- Do not have heavy menstrual bleeding on the day of test
The painless, simple, and quick HPV test can be performed by yourself in a healthcare setting, usually in a bathroom or toilet.
A package that consists of a swab will be given to you.
You will have to gently insert the swab into your vagina (similar to inserting a tampon).
Then, rotate the swab 5-10 times.
When you are done, remove the swab and place it back in the tube without cleaning and dropping it.
After your HPV test, you can go about your day without restrictions. You may also perform the HPV test at any time as long as you are not having heavy menstrual bleeding.
- HPV is not detected in the sample (everything is normal).
- This implies that your risk of developing abnormal cell changes in the cervix is extremely low. Your next cervical screening HPV test can be repeated after 5-10 years.